Endometrial Carcinoma represents about 5% of female cancers worldwide. In 2022, there were 420,368 new cases of endometrial carcinoma recorded globally. Among these patients, about 3% were aged between 15 and 44 years (Globocan 2022)
From January 2021 to December 2023, 100 patients with an initial diagnosis of endometrial cancer and atypical complex hyperplasia (39 endometrial cancer and 61 atypical complex hyperplasia) were conservatively treated by Dr. Catena at the CLASS Hysteroscopy center of the Policlinico Universitario Agostino Gemelli IRCCS of Rome.
In the last decade, the average age of women at their first pregnancy has been around 35-39 years, with more women having their first pregnancy after 40.
Therefore, it is increasingly important to provide young women with a diagnosis of endometrial carcinoma, who desire children, with a personalized path that supports and guides them to pregnancy as soon as their treatment response is complete.
Another interesting aspect is that this condition often occurs in young obese women. Hence, there is a need for a multidisciplinary and personalized approach, with a care plan tailored to each individual patient.
In women aged 40 years or younger, low-grade and low-stage neoplasms are more frequently found.
The ESGO/ESHRE/ESGE guidelines (ESGO: European Society of Gynaecological Oncology, ESHRE: European Society of Human Reproduction and Embryology, ESGE: European Society for Gynaecological Endoscopy) published in January 2023 define fertility-sparing treatment for endometrial carcinoma as a treatment outside the standard of care. The recommended treatment involves radical surgical intervention (total hysterectomy + bilateral salpingo-oophorectomy + surgical staging), but this would obviously deny these women the opportunity to fulfill their desire for motherhood.
The ESGO/ESHRE/ESGE guidelines state that the best fertility-sparing treatment consists of complete hysteroscopic resection of the tumor followed by progestin therapy.
Obviously, strict and well-defined eligibility criteria for such patients for conservative treatment must be adopted, along with appropriate counseling, emphasizing that fertility-sparing surgery is outside the standard of care and should be reserved for women with a strong reproductive desire, who, once exhausted, may then undergo radical surgery. This creates the need for a correct path to guide the patient, ensuring proper follow-up, as this process will involve fertility-sparing primary surgery, medical therapy, pregnancy pursuit, and subsequent radical surgery once the reproductive desire has been fulfilled.
This process must consider some key factors:
• Patient eligibility for treatment
• The type of treatment to administer
• Treatment response
• Follow-up
• Reproductive outcomes
ELIGIBILITY
To consider a patient eligible for conservative treatment, we must evaluate certain aspects:
• A fertile-age patient with a strong desire for pregnancy
• Disease grade
• Disease stage
• Histotype
According to ESGO/ESHRE/ESGE guidelines, we must deal with a well-differentiated endometrioid adenocarcinoma (G1). The disease must be limited to the endometrium, without signs of myometrial invasion or cervical extension, and without ovarian pathology, pelvic/paraaortic lymphadenopathy, or distant metastases.
Patients must not have contraindications to hormonal medical therapy or pregnancy.
Such patients must always undergo PELVIC ULTRASOUND and PELVIC MRI WITH AND WITHOUT CONTRAST AGENT. They must also undergo OUTPATIENT DIAGNOSTIC HYSTEROSCOPY WITH ENDOMETRIAL BIOPSY.
TREATMENT TYPE
Fertility-sparing hysteroscopic surgery is a fundamental aspect of the therapy's success and must be personalized based on the endometrial lesion found in the uterus.
Thus, outpatient hysteroscopy with endometrial biopsy is the diagnostic method recommended by the ESGO/ESHRE/ESGE guidelines, as it not only provides the endometrial material for analysis but also allows for description of the type of endometrial lesion that must be treated.
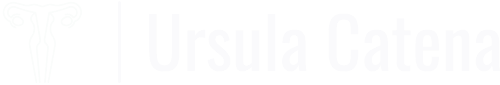
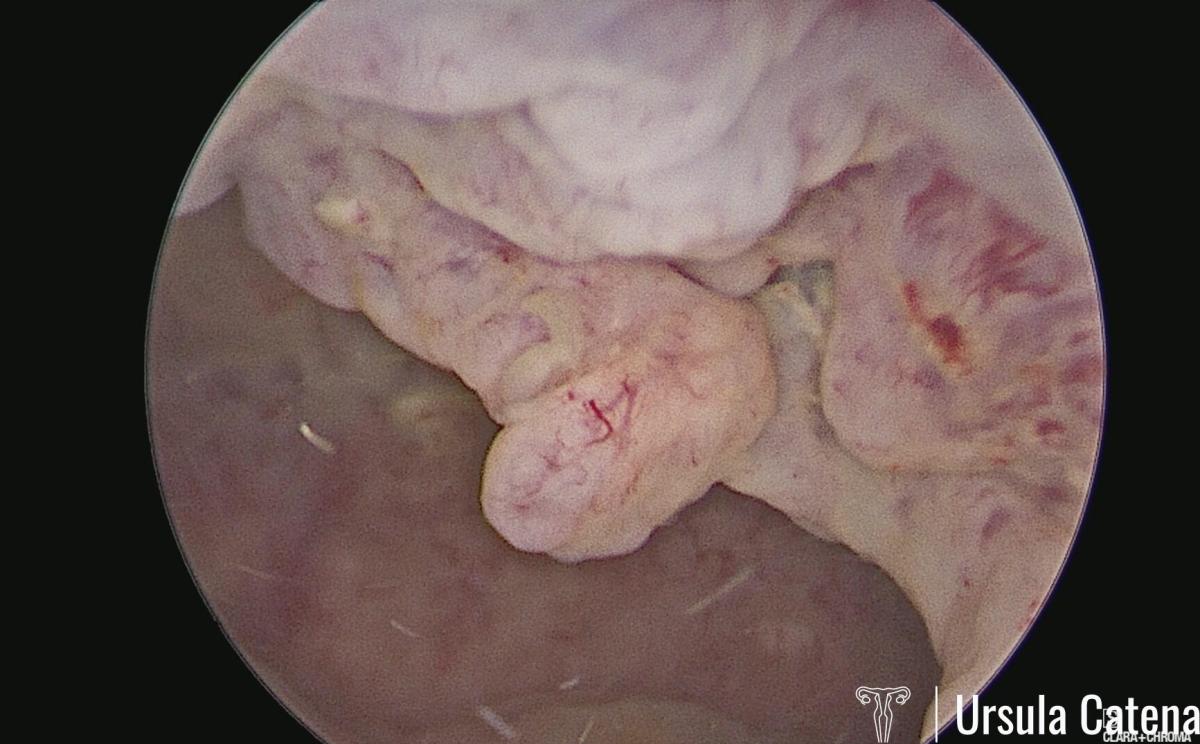
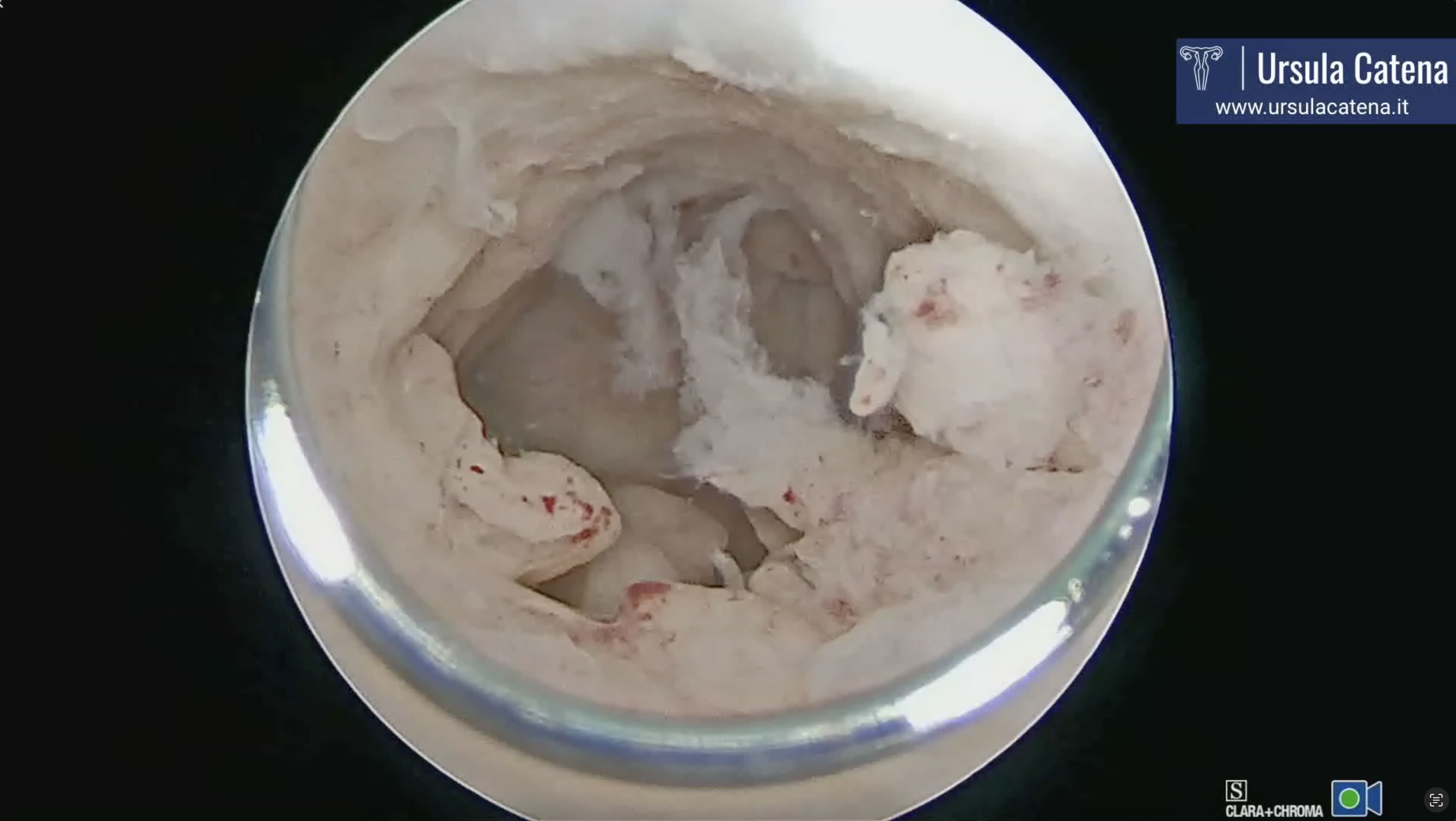
In case of a focal lesion, a hysteroscopic resection technique, first proposed by the Italian Ivan Mazzon in 2005, is used. This technique involves three steps: 1) removal of the endometrial lesion; 2) removal of the endometrium adjacent to the lesion; 3) removal of the myometrium beneath the lesion. Due to the evolution of hysteroscopic technologies, this procedure is now performed with miniaturized instruments (bipolar miniresectoscope 15Fr - 5mm), avoiding cervical canal dilation (see video: focal cancer). This approach reduces the risk of possible complications (especially uterine perforation) and minimizes the risk of intrauterine adhesions post-surgery, which is crucial for achieving pregnancy after a complete response to treatment.
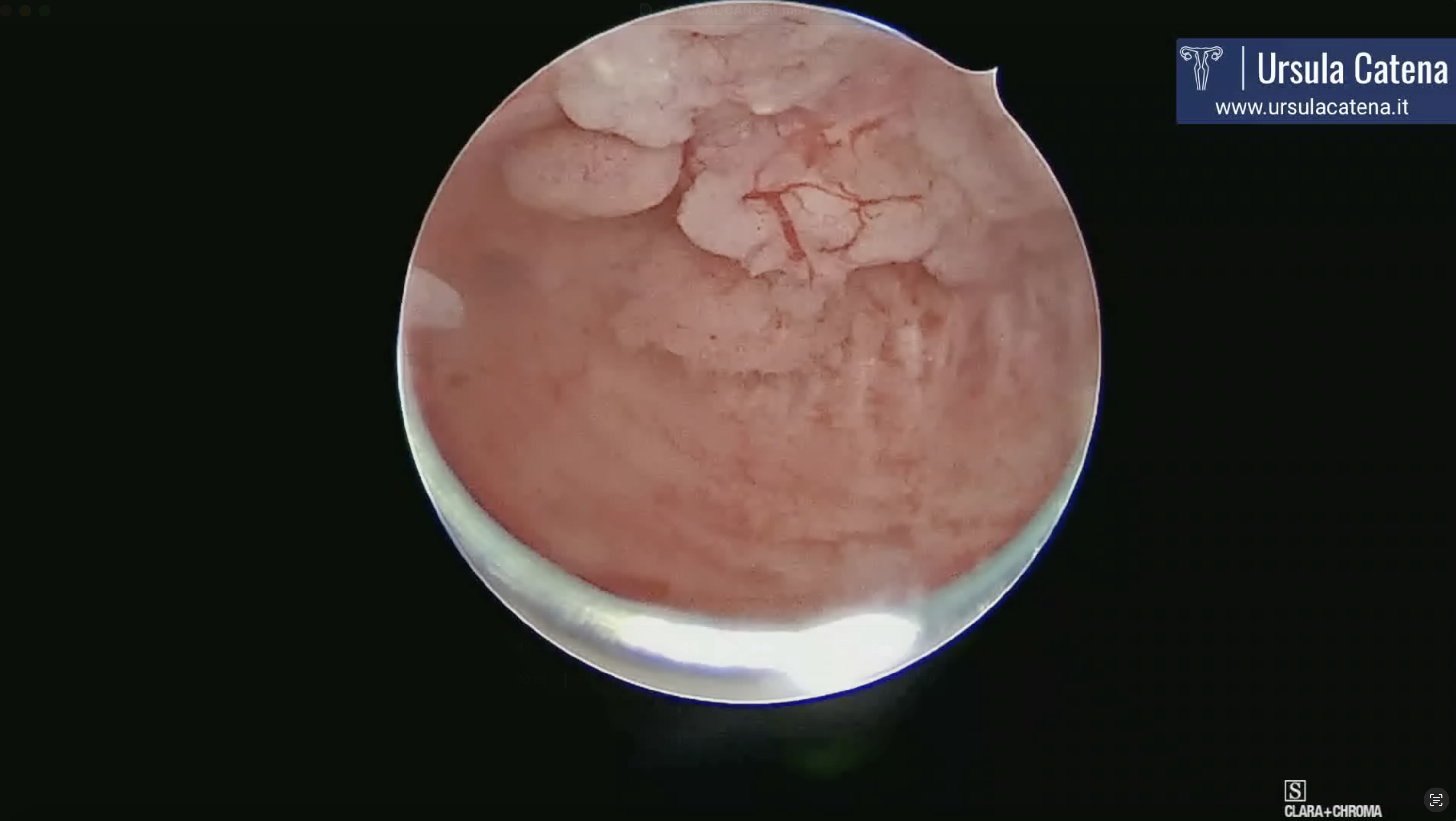
In case of atypical endometrial hyperplasia, a technique called visual D&C is performed, first described by Paolo Casadio in 2022. This technique uses an innovative tool, the Tissue Removal Device (TRD), which simultaneously "grinds and aspirates" tissue. This tool is entirely mechanical, so it does not require energy use within the uterine cavity. For these reasons, it is very safe both in terms of preventing intra- and post-operative complications and in terms of preventing intrauterine adhesions (see video: visual D&C).
In case of diffuse cancer, a technique described by Ursula Catena's team in 2023 is used. This involves using the bipolar miniresectoscope 15Fr on major lesions up to the myometrial plane, followed by the use of TRD to complete endometrial resection in more delicate areas such as near the tubal ostia and, in any case, to avoid energy use throughout the entire uterine cavity and thus prevent possible post-operative intrauterine adhesions (see video: Diffuse Cancer & 3 months Control).
Moreover, operative hysteroscopy ensures the availability of tissue for immunohistochemical analysis of the tumor, a new frontier for evaluating genetic risk in these patients.
The ESGO/ESHRE/ESGE guidelines recommend using a progestin-based medical therapy, either orally or via intrauterine devices (IUDs) medicated with Levonorgestrel (LNG). Literature suggests a complete response rate exceeding 95% for hysteroscopic resection followed by progestin therapy, compared to around 70-75% for the use of progestins alone (oral or local).
Additionally, it has been shown that the use of the LNG IUD has a lower recurrence rate (11%) compared to oral progestins (30.7%) (Fan et al. 2018).
Our protocol therefore includes the immediate insertion of the LNG IUD after endometrial resection.
In cases of atypical complex hyperplasia or endometrioid G1 endometrial adenocarcinoma, therapy will involve the sole use of LNG IUD. In cases of endometrioid G1 MMRd or G2 MMRp endometrial adenocarcinoma, oral progestin (Megestrol acetate 160 mg/day) will be added, as it has been shown that the combination of both progestins results in a higher complete response rate.
TREATMENT RESPONSE AND FOLLOW-UP
Patients will undergo OUTPATIENT HYSTEROSCOPY + ENDOMETRIAL BIOPSY every 3 months.
Every 6 months, they will undergo PELVIC ULTRASOUND and CA 125 testing.
REPRODUCTIVE OUTCOMES
When the patient achieves a complete response (CR) and maintains it for 6 months (2 consecutive negative endometrial biopsies), pregnancy pursuit is encouraged. Pregnancy rates for different techniques (oral progestin therapy only; hysteroscopic resection + LNG-IUD; LNG-IUD only) are around 50% for treated patients.
FERTILITY-SPARING TREATMENT IN OBESE PATIENTS
As previously mentioned, many patients with endometrial carcinoma or its precursors (atypical complex hyperplasia) are obese. Obesity and the associated metabolic conditions (hyperestrogenism, metabolic syndrome, peripheral insulin resistance, diabetes) are considered risk factors for the development of endometrial cancer. Special attention must therefore be given to this subgroup of women.
Eligibility criteria for conservative treatment are the same as for the general population (early-stage, low-grade tumors), following thorough evaluation with pelvic ultrasound and MRI. The proposed treatment consists of conservative removal of endometrial pathology through hysteroscopy, combined with oral and local hormonal therapy. It is important to note that although the therapies are the same, some authors have noted that response rates in obese patients are lower compared to normal-weight patients, and their obstetric success rate is also lower.
Combining a therapy that can address the metabolic alterations typical of obesity has shown a synergistic effect in treating endometrial conditions in obese patients. Specifically, the combination with metformin has shown an improvement in the long-term response to hormonal therapy.
Additionally, weight loss programs combined with the aforementioned therapy are currently being studied.
Among the many weight loss techniques, in addition to balanced diet plans from expert nutritionists and medical therapy, invasive surgical techniques like traditional bariatric surgery and endoscopic techniques like vertical gastroplasty should be mentioned. It has been described that in obese patients undergoing bariatric surgery, the risk of developing endometrial cancer is reduced by about 60%.
Therefore, a multidisciplinary approach involving gynecologists, bariatric surgeons/digestive endoscopists, nutritionists, endocrinologists, and psychologists is essential for optimal treatment of obese patients with endometrial abnormalities.
FUTURE PERSPECTIVES
At the CLASS Hysteroscopy center, as part of research protocols, we offer combined hysteroscopic + progestin medical therapy to patients with stage IA G2 endometrial carcinoma and to patients with stage IA G1 endometrial carcinoma with minimal myometrial infiltration, with encouraging results, also in line with the new ESGO/ESHRE/ESGE guidelines. Standardizing the treatment pathway and including patients in a well-structured and defined program enables us to design prospective clinical trials for increasingly complex patients.
Moreover, recent results from molecular analysis to assess genetic risk in these patients have shown promising results. Therefore, we have introduced endometrial molecular analysis in the evaluation of young patients undergoing conservative treatment to further personalize treatment for each individual patient.
Look our photos
Look our videos